✅Case 1:
Patient: 45-year-old male
Symptoms:
- Vertigo induced by loud sounds (Tullio phenomenon)
- Autophony (hears own voice echoing loudly)
- Dizziness with pressure changes
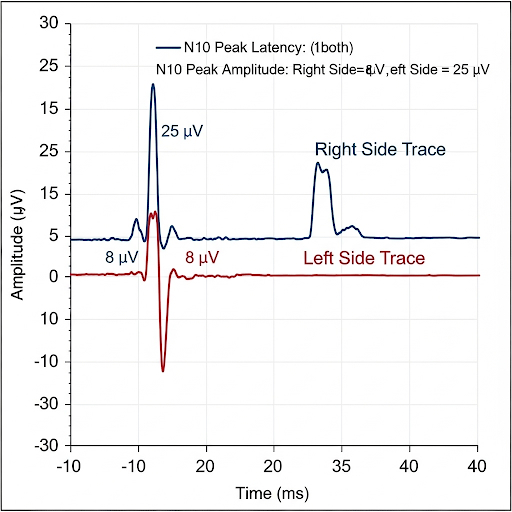
oVEMP Results:
- Stimulus: Air-conducted sound (ACS, 500 Hz tone burst)
- Findings:
- Abnormally large amplitude n10 response on the affected (left) side
- Normal latency but much higher than normal amplitude (e.g., 25 µV vs. <10 µV typical)
- Right side normal amplitude
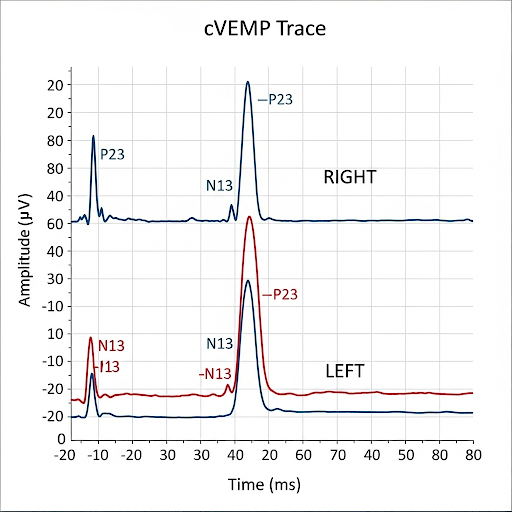
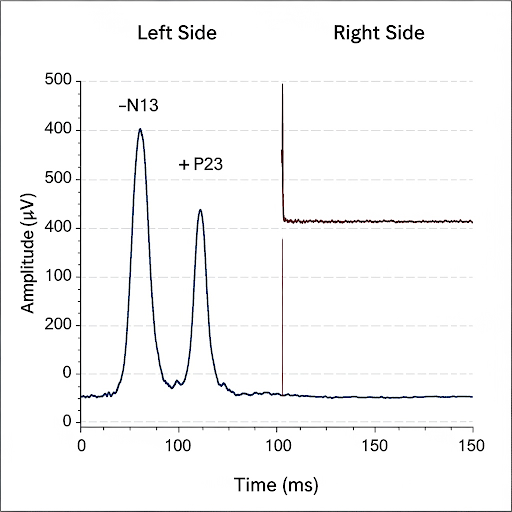
cVEMP Results (same patient):
- Lower than normal threshold (VEMP present at 70 dB nHL, instead of 85–95 dB)
- Robust amplitude response in the left sternocleidomastoid muscle
Conclusion:
The enhanced oVEMP amplitude and low-threshold cVEMP strongly point to Superior Canal Dehiscence Syndrome (SCDS).
✅Case 2:
Patient: 60-year-old female
Symptoms:
- Acute vertigo episode 3 weeks ago, lasting days
- Persistent imbalance but no hearing loss
- No sound- or pressure-induced vertigo
cVEMP Results:
- Stimulus: 500 Hz tone burst
- Findings:
- Absent cVEMP response on the right side (ipsilateral SCM)
- Normal, robust cVEMP response on the left side
- Indicates saccule/inferior vestibular nerve dysfunction on the right
oVEMP Results (same patient):
- Normal n10 responses bilaterally
- Suggests utricle/superior vestibular nerve intact
Conclusion:
The unilateral absent cVEMP with normal oVEMP indicates an inferior vestibular nerve lesion on the right, consistent with Vestibular Neuritis (inferior branch involvement).
.
✅Case 3:
Patient: 52-year-old male
Symptoms:
- Progressive unilateral hearing loss (right ear)
- Tinnitus (right ear)
- Occasional imbalance
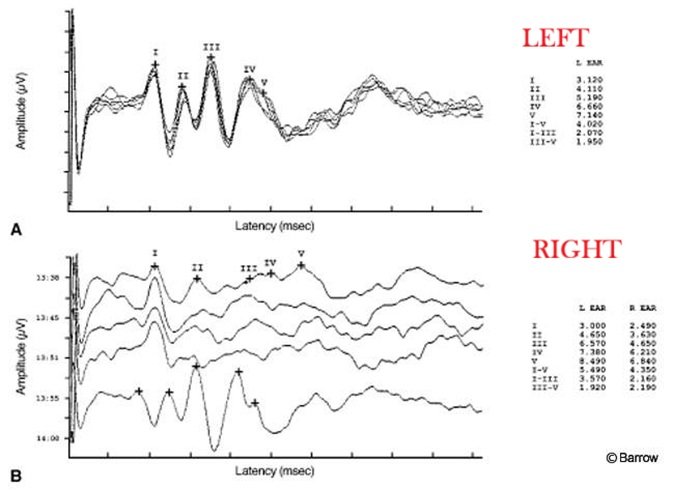
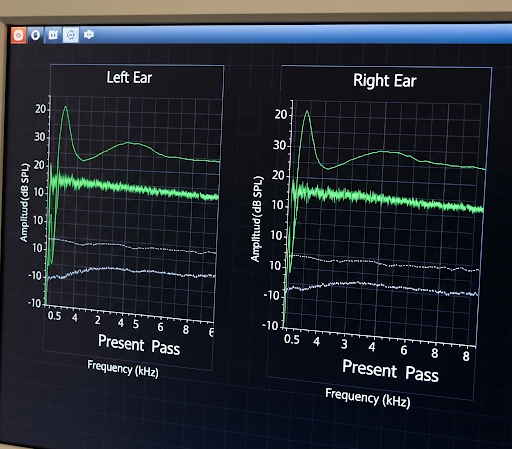
ABR Results:
- Right Ear:
- Wave I: Present, normal latency
- Wave III: Delayed
- Wave V: Markedly delayed (interaural Wave V latency difference >0.4 ms)
- Interpeak intervals (I–III and I–V) prolonged
- Reduced Wave V amplitude compared to left ear
- Left Ear: Normal absolute and interpeak latencies
Conclusion:
These findings suggest a retrocochlear lesion, most consistent with Acoustic Neuroma (Vestibular Schwannoma) on the right side.
✅Case 4:
Patient: 4-year-old female
Symptoms:
- Delayed speech and language development
- Parents report she “hears sometimes but not clearly”
- Normal otoacoustic emissions (OAE)
ABR Results:
- Click stimulus:
- No clear, replicable waves (I–V) present in either ear
- Neural synchrony absent (very poor waveform morphology)
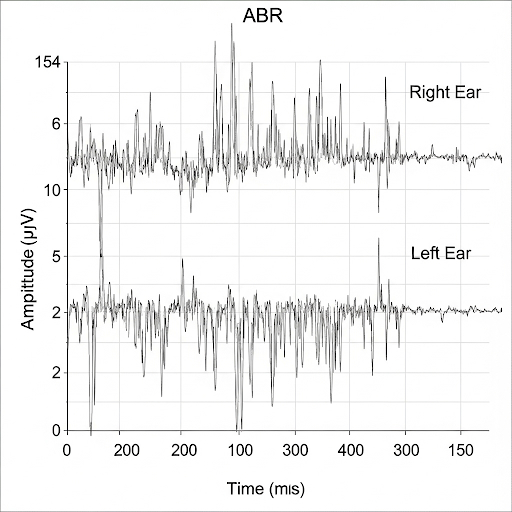
- Cochlear Microphonic (CM):
- Present and normal
- OAE: Present and normal
Conclusion:
The combination of present OAEs/cochlear microphonic with absent/abnormal ABR waves is diagnostic of Auditory Neuropathy Spectrum Disorder (ANSD), reflecting disrupted neural transmission despite intact outer hair cell function.
✅Case 5:
Patient: 2-month-old infant (newborn hearing screening referral)
History:
- No family history of hearing loss
- Passed OAE in one ear, referred in the other
- Parents concerned about lack of startle response to sound
ABR Results:
- Click stimulus, both ears:
- No identifiable ABR waves (I–V) up to 90 dB nHL
- Tone-burst ABR:
- No response at 500, 1000, 2000, or 4000 Hz (both ears)
- OAE: Absent bilaterally
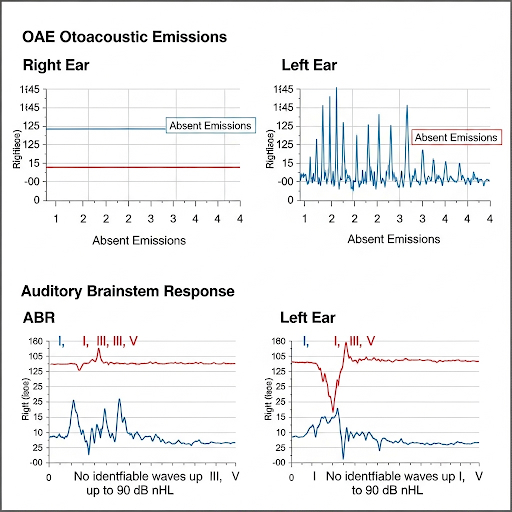
Interpretation:
Absence of all ABR waves with absent OAEs suggests severe-to-profound bilateral sensorineural hearing loss (SNHL), likely congenital in nature.
Conclusion:
Diagnosis: Congenital Bilateral SNHL → early intervention (hearing aids, possible cochlear implant candidacy).
✅Case 6:
Patient: 1-week-old premature infant (NICU)
History:
- Complicated birth, low Apgar scores, required resuscitation
- Risk factor: hypoxic-ischemic encephalopathy
- Passed OAE screening
ABR Results:
- Both ears:
- Wave I: Present, normal latency
- Wave III: Poor morphology, delayed
- Wave V: Absent or extremely delayed
- Interpeak latencies (I–III and III–V) prolonged
- OAE: Present bilaterally
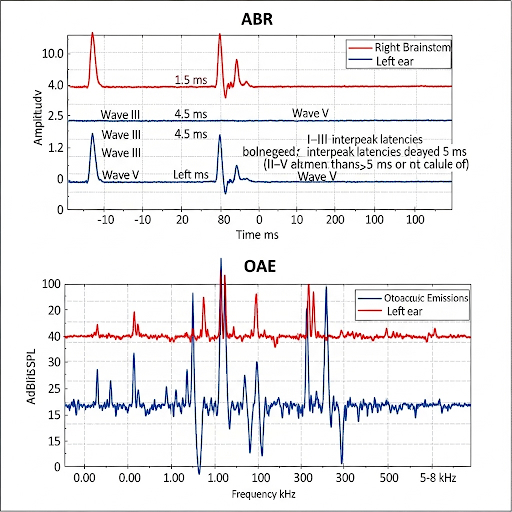
Interpretation:
- Cochlear function intact (OAE present, Wave I present)
- Neural transmission through the brainstem abnormal (delayed/absent waves III–V)
- Suggests central auditory pathway dysfunction due to hypoxic brain injury.
Conclusion:
Diagnosis: Hypoxic-Ischemic Encephalopathy (HIE) with auditory brainstem involvement → prognosis depends on neurological recovery.
✅Case 7:
Patient: 68-year-old female
History:
- Reports sudden vertigo when rolling over in bed to the right side
- No hearing loss, no tinnitus
- Vertigo lasts seconds, accompanied by nausea
- No recent infections, but had minor fall 2 weeks ago
Test Findings (Dix-Hallpike):
- Right ear down position:
- Latency: 2–3 seconds before onset
- Torsional up-beating nystagmus observed
- Nystagmus fatigues within ~20 seconds
- Left ear down position: No abnormal response
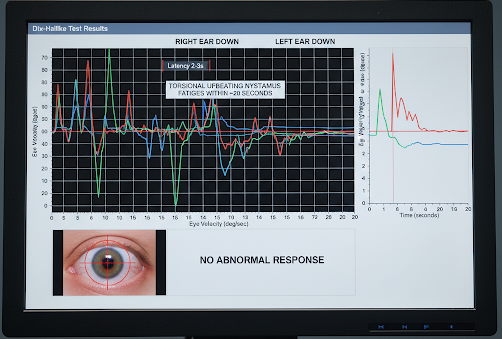
Interpretation:
The up-beating torsional nystagmus on right Dix-Hallpike is characteristic of posterior canal BPPV on the right side.
Conclusion:
Diagnosis: Right Posterior Canal BPPV → managed with Epley repositioning maneuver.
✅Case 8:
Patient: 55-year-old male
History:
- Dizziness triggered by turning head quickly in bed
- No hearing loss, no tinnitus
- Vertigo more intense when lying on the left side
Test Findings (Supine Roll Test):
- Head turned to left:
- Geotropic (toward the ground) horizontal nystagmus
- Stronger response on the left side
- Head turned to right:
- Geotropic horizontal nystagmus but weaker than left
Interpretation:
- Geotropic nystagmus indicates canalithiasis
- Stronger response when head is turned toward the affected ear
- Therefore, left horizontal canal BPPV (geotropic variant)
Conclusion:
Diagnosis: Left Horizontal Canal BPPV (Geotropic Type) → managed with Barbecue (Lempert) roll maneuver.
✅Case 9:
Patient: 62-year-old male
History:
- Long history of intravenous antibiotics (gentamicin) for recurrent infections
- Complains of chronic unsteadiness, especially in the dark or when walking on uneven ground
- Reports oscillopsia (blurry vision during head movements)
- No tinnitus or hearing loss
Test Findings:
- Head Impulse Test (HIT): Abnormal, bilaterally (catch-up saccades seen)
- Dynamic Visual Acuity (DVA): Markedly reduced
- Caloric Testing: Bilateral reduced/absent responses
- Rotary Chair: Low gain, reduced phase lead — bilateral vestibular weakness
- cVEMP & oVEMP: Absent bilaterally
Interpretation:
Absent/abnormal vestibular responses across multiple tests confirm bilateral vestibular hypofunction, most consistent with ototoxic injury.
Conclusion:
Diagnosis: Bilateral Vestibulopathy due to Aminoglycoside (Gentamicin) Ototoxicity → requires vestibular rehabilitation and fall-prevention strategies.
✅Case 10:
Patient: 38-year-old female
History:
- Recurrent episodes of vertigo lasting hours, often with migraine headaches
- Associated photophobia, phonophobia, nausea
- Triggers: stress, certain foods, hormonal fluctuations
- No hearing loss, no tinnitus
- Family history of migraine
Test Findings:
- VNG (Videonystagmography): May show nonspecific findings; calorics within normal limits
- VEMP (cVEMP/oVEMP): Normal
- ABR: Normal
- MRI: No vestibular pathology
- Clinical history strongly fulfills ICHD-3 criteria for vestibular migraine
Interpretation:
Vestibular tests often appear normal, but the clinical history and migraine association are key.
Conclusion:
Diagnosis: Vestibular Migraine → treated with migraine prophylaxis (diet/lifestyle modifications, medications such as beta-blockers or calcium-channel blockers).
✅Case 11:
Patient: 22-year-old university student
History:
- Sustained a concussion after a soccer collision (head-to-head impact).
- Symptoms: Headache, dizziness, blurred vision, difficulty concentrating, imbalance, and occasional tinnitus.
- No loss of consciousness, no skull fracture.
Test Results
Pure-Tone Audiometry (PTA):
- Thresholds: Within normal limits (0–20 dB HL across frequencies bilaterally).
- Slight difficulty reported with hearing in noisy environments (possible central auditory processing involvement rather than peripheral hearing loss).
Auditory Brainstem Response (ABR):
- Absolute latencies of Waves I, III, V: Within normal range.
- Interwave intervals: Slight prolongation of III–V bilaterally (suggesting possible brainstem conduction delay, consistent with diffuse axonal injury often seen in concussion).
- Overall interpretation: Subtle central auditory pathway involvement, despite normal PTA.
Bedside Vestibular/Balance Tests:
- Head impulse test (HIT): Negative (VOR intact).
- Romberg test: Patient sways significantly with eyes closed, nearly loses balance.
- Tandem gait: Difficulty maintaining a straight line.
- Dix-Hallpike maneuver: Negative for positional vertigo (rules out BPPV).
Instrumented Vestibular Testing (if performed):
- VNG (ocular motor): Slight abnormalities in smooth pursuit and saccades → central involvement.
- Posturography: Increased sway area in sensory organization test conditions that rely on vestibular input.
Conclusion:
This patient presents with a concussion-related central vestibular dysfunction.
- Hearing per se is intact (normal PTA).
- ABR shows subtle brainstem conduction delays, suggesting central auditory pathway effects.
- Balance tests point to vestibular and proprioceptive integration issues, typical after concussion.
✅Case 12:
Patient: 35-year-old construction worker
History:
- Fell at work, struck head lightly against a wall.
- Diagnosed with mild concussion in ER.
- Current complaints: brief episodes of spinning vertigo triggered by lying down, rolling over in bed, or looking up.
- No hearing loss or tinnitus.
Bedside Balance / Vestibular Results:
- Romberg test: Stable with eyes open and closed.
- Tandem gait: Performed without significant difficulty.
- Head impulse test (HIT): Negative (VOR intact).
- Dix-Hallpike maneuver:
- Right ear down: Delayed onset (2–3 sec), brief torsional/upbeating nystagmus, lasting ~15 sec → positive.
- Left ear down: Negative.
- Head-shake test: No spontaneous nystagmus observed.
Conclusion:
This patient’s balance findings are consistent with post-traumatic BPPV (right posterior canal).
- Unlike the previous concussion case with central signs (Romberg sway, abnormal smooth pursuit),
- Here the bedside results point to a peripheral positional vestibular disorder.
✅Case 13:
Patient: 50-year-old male
History:
- Sudden onset severe vertigo, nausea, vomiting, and unsteady gait.
- No hearing loss, no tinnitus.
- Symptoms started abruptly 12 hours ago.
VNG (Videonystagmography) Results:
Spontaneous Nystagmus:
- Left-beating horizontal nystagmus, present at rest, increases when fixation removed.
Gaze-Evoked Nystagmus:
- Mild, horizontal, toward the left; decreases with fixation.
Positional Testing:
- Dix-Hallpike: Negative bilaterally → no BPPV.
Head-Shake Test:
- Exaggerated nystagmus to the left after horizontal head-shake.
Caloric Testing:
- Right ear: 90% hypofunction (canal paresis)
- Left ear: Normal response
Oculomotor Testing:
- Smooth pursuit: Normal
- Saccades: Normal
Interpretation / Conclusion:
- Acute right-sided vestibular neuritis (peripheral vestibular lesion).
- Severe vertigo, spontaneous nystagmus, and canal paresis on calorics confirm unilateral vestibular hypofunction.
- Normal oculomotor tests support peripheral rather than central cause.
- Treatment: Vestibular suppressants short-term, vestibular rehabilitation therapy, and follow-up for compensation.
✅Case 14:
- Age/Gender: 45-year-old male
- Presenting Complaint: Persistent dizziness and imbalance following a motor vehicle accident 3 months ago.
- Medical History: No significant prior medical history. No loss of consciousness at the time of the accident.
Clinical Findings:
- Physical Examination: Mild unsteadiness observed during tandem gait; no significant abnormalities noted in other neurological examinations.
- Audiological Assessment: Normal pure-tone audiometry; no significant findings on videonystagmography.
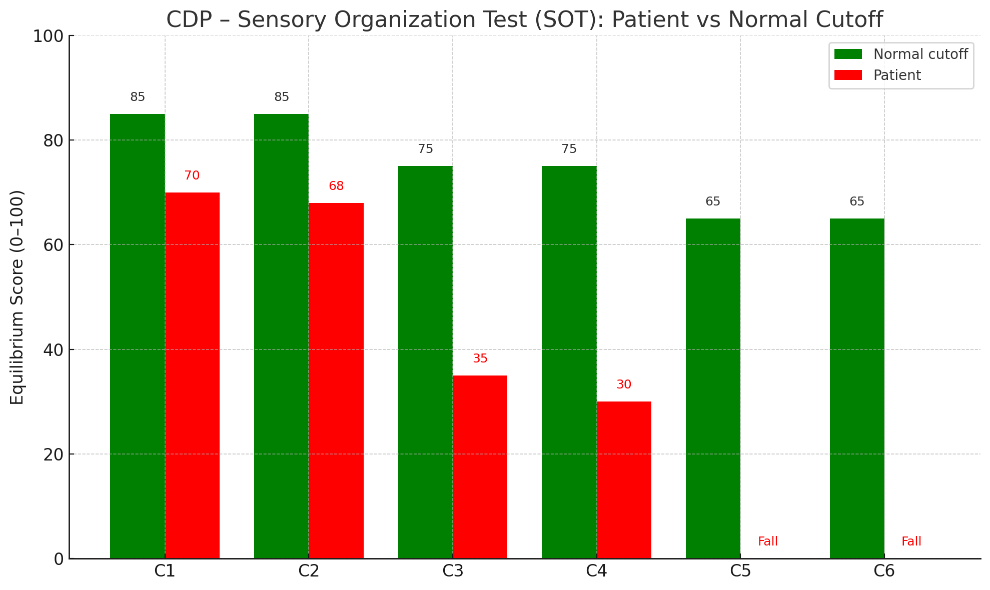
CDP Results:
Sensory Organization Test (SOT):
- Condition 1 (eyes open, stable surface): 100% stability.
- Condition 2 (eyes closed, stable surface): 85% stability.
- Condition 3 (eyes open, sway-referenced surface): 75% stability.
- Condition 4 (eyes closed, sway-referenced surface): 50% stability.
- Condition 5 (eyes open, sway-referenced visual surround): 60% stability.
- Condition 6 (eyes closed, sway-referenced visual surround): 30% stability.
- Interpretation: Significant deficits in conditions that challenge visual and somatosensory inputs, indicating impaired sensory integration.
Motor Control Test (MCT):
- Condition 1 (fixed surface): 90% stability.
- Condition 2 (sway-referenced surface): 60% stability.
- Interpretation: Difficulty maintaining balance on a sway-referenced surface, suggesting impaired motor control.
Adaptation Test (ADT):
- Condition 1 (eyes open, fixed surface): 95% stability.
- Condition 2 (eyes closed, fixed surface): 85% stability.
- Condition 3 (eyes open, sway-referenced surface): 70% stability.
- Condition 4 (eyes closed, sway-referenced surface): 40% stability.
- Interpretation: Impaired ability to adapt to changing postural conditions, particularly when visual inputs are removed.
Diagnosis:
- Primary: Post-concussion syndrome with vestibular dysfunction.
- Secondary: Impaired sensory integration and motor control.
✅Case 15:
Patient:
- Age/Gender: 38-year-old female
- Presenting Complaint: Persistent imbalance and dizziness following a viral upper respiratory infection 6 months ago.
- Medical History: No significant prior medical history. No history of head trauma or ototoxic drug use.
Clinical Findings:
- Physical Examination: Mild unsteadiness observed during tandem gait; no significant abnormalities noted in other neurological examinations.
- Audiological Assessment: Normal pure-tone audiometry; no significant findings on video nystagmography.
Rotary Chair Testing Results:
- Sinusoidal Harmonic Acceleration (SHA) Test:
- Low Frequency (0.01–0.08 Hz): Reduced gain and phase lead, indicating impaired vestibulo-ocular reflex (VOR).
- Mid Frequency (0.1–0.64 Hz): Significantly reduced gain, with phase abnormalities.
- High Frequency (0.8–1.28 Hz): Markedly reduced gain, with phase abnormalities.
- Symmetry: Asymmetric responses, with greater impairment on the left side.
- Interpretation: Bilateral vestibular hypofunction, with more pronounced impairment on the left side.
- Step Velocity Test:
- Leftward Rotation: Reduced VOR gain with prolonged time constant, indicating impaired semicircular canal function.
- Rightward Rotation: Reduced VOR gain with prolonged time constant, indicating impaired semicircular canal function.
- Interpretation: Bilateral impairment of semicircular canal function.
Diagnosis:
- Primary: Bilateral vestibular hypofunction, likely post-viral in origin.
✅Case 16:
- Age/Gender: 47-year-old female
- Presenting Complaint: Recurrent episodes of vertigo lasting 20–60 minutes, fluctuating hearing loss in the left ear, tinnitus (“roaring” sound), and aural fullness.
- History: Symptoms started ~2 years ago, episodic, worsening over time.
Main Balance Test Results
Bedside Vestibular Tests:
- Romberg Test: Sways to the left during eyes closed condition.
- Tandem Gait: Mild instability, especially during acute attacks.
- Head Impulse Test: Normal between attacks; may show hypofunction during acute vertigo.
- Dix-Hallpike: Negative (rules out BPPV).
Videonystagmography (VNG):
- Spontaneous Nystagmus: Occasionally left-beating during acute attacks.
- Positional Nystagmus: Mild positional nystagmus noted toward the affected ear.
- Ocular Motor Tests: Normal between attacks.
Caloric Testing:
- Left ear: Reduced response (canal paresis 40–50%).
- Right ear: Normal response.
- Interpretation: Unilateral vestibular hypofunction corresponding to symptomatic ear.
Computerized Dynamic Posturography (CDP):
- Sensory Organization Test (SOT):
- Reduced stability in conditions relying on vestibular input (conditions 5 & 6).
- Sway increased during eyes closed and sway-referenced visual conditions.
Conclusion:
- Diagnosis: Left-sided Ménière’s disease.
- Balance Profile: Intermittent unilateral vestibular hypofunction with central compensation between attacks, mild postural instability on dynamic balance tests, and acute peripheral vestibular signs during vertigo episodes.
✅Case 17:
- Age/Gender: 62-year-old male
- Presenting Complaint: Sudden onset of severe dizziness, unsteady gait, nausea, vomiting, and difficulty coordinating movements.
- History: Hypertension and type 2 diabetes; no prior vestibular issues.
Balance Test Results
Bedside Vestibular/Neurological Tests:
- Romberg Test: Marked sway, falls toward the right side; cannot maintain stance with eyes closed.
- Tandem Gait: Unable to perform; falls to the right.
- Finger-to-Nose / Heel-to-Shin: Dysmetria on right side.
- Rapid Alternating Movements: Dysdiadochokinesia on right.
- Head Impulse Test (HIT): Normal (suggests central, not peripheral, vestibular lesion).
Videonystagmography (VNG):
- Spontaneous Nystagmus: Vertical or direction-changing gaze-evoked nystagmus, present with fixation removed.
- Oculomotor Tests:
- Saccades: Dysmetric (overshoot/undershoot)
- Smooth pursuit: Poor tracking, saccadic intrusions
- Positional Testing: No positional nystagmus (rules out BPPV)
Computerized Dynamic Posturography (CDP):
- Sensory Organization Test (SOT):
- Condition 1 & 2 (stable surface): Mild instability
- Condition 3–6 (sway-referenced surface or visual surround, eyes closed): Severe instability
- Falls or near-falls in conditions 5 & 6
- Interpretation: Severe impairment in integrating vestibular and somatosensory input, consistent with cerebellar dysfunction.
Romberg + Foam Surface:
- Patient loses balance rapidly, especially with eyes closed, confirming reliance on visual input and poor central integration.
Conclusion:
- Diagnosis: Right cerebellar infarct affecting vestibulocerebellum- Cerebellar Stroke (Right Hemisphere)
- Balance Profile: Severe postural instability, dysmetria, dysdiadochokinesia, and central oculomotor deficits.
- Clinical Significance: Central cause of imbalance; high fall risk; requires acute neurological care and long-term vestibular/cerebellar rehabilitation.
✅Case 18:
Patient: 62-year-old male
History: Complains of chronic unsteadiness when walking, worse in the dark or on uneven ground. Reports oscillopsia (blurred vision when moving head). No true spinning vertigo, but severe imbalance that has gradually worsened. History of gentamicin IV treatment for sepsis 1 year ago.
Audiologic/Vestibular Symptoms:
- Difficulty walking without visual cues
- Oscillopsia during head movement
- No significant hearing loss reported
- Positive Romberg with eyes closed
Caloric Test Results (Bithermal, water irrigation)
| Ear | Warm (°/sec) | Cool (°/sec) |
| Right | 1°/sec | 0°/sec |
| Left | 0°/sec | 1°/sec |
Total responses: 2°/sec (severe bilateral hypofunction)
- Normal total response: >20°/sec
- This patient: essentially bilateral caloric areflexia
Conclusion
The results show bilateral vestibular loss, consistent with bilateral vestibular hypofunction most likely secondary to ototoxicity from aminoglycosides (gentamicin toxicity).
This explains the oscillopsia, imbalance, and absent caloric responses.
✅Case 19:
Patient: 34-year-old female
History: Reports recurrent dizziness episodes triggered by stress, poor sleep, and during migraine attacks. Describes rocking/floaty imbalance rather than true spinning vertigo. Symptoms worsen in visually complex environments (e.g., grocery stores). Strong history of migraine with aura and generalized anxiety disorder.
Audiologic/Vestibular Symptoms:
- Imbalance and unsteadiness, worse with stress or visual motion
- Photophobia and phonophobia during migraine episodes
- No significant hearing loss or tinnitus
- Anxiety significantly worsens perception of dizziness
Caloric Test Results (Bithermal, water irrigation)
| Ear | Warm (°/sec) | Cool (°/sec) |
| Right | 18°/sec | 22°/sec |
| Left | 20°/sec | 21°/sec |
Total response: 81°/sec (within normal limits)
- No significant unilateral weakness (<20% difference)
- Normal directional preponderance (<25%)
- Symmetrical and robust responses
Conclusion
The caloric test results are normal, which is typical for MARDD. Despite normal peripheral vestibular function, the patient’s dizziness stems from a central migraine/anxiety interaction and altered sensory integration, not from peripheral vestibular hypofunction.
✅Case 20:
Patient: 10-year-old boy
History: Presented with recurrent episodes of vertigo, nausea, and imbalance for the past 6 months. Parents report fluctuating hearing loss and occasional tinnitus in the left ear. School performance is affected due to frequent absences. No history of head trauma or ototoxic medications.
Audiologic/Vestibular Symptoms:
- Fluctuating unilateral (left-sided) hearing loss
- Recurrent vertigo attacks lasting 1–2 hours
- Aural fullness in the left ear
- Difficulty participating in sports due to imbalance
Electrocochleography (EcoG) Test Results
Stimulus: Clicks at 90 dB nHL, transtympanic recording
| Parameter | Right Ear (normal) | Left Ear (affected) |
| Summating Potential (SP) amplitude | 0.08 µV | 0.22 µV |
| Action Potential (AP) amplitude | 0.38 µV | 0.32 µV |
| SP/AP Ratio | 0.21 (normal) | 0.69 (abnormal, >0.45) |
Conclusion
The EcoG results show an elevated SP/AP ratio in the left ear, consistent with endolymphatic hydrops. Combined with fluctuating hearing loss, vertigo, and aural fullness, this suggests pediatric Ménière’s disease (rare but possible in children).
✅Case 21:
Female, 36 years old
Gradual hearing loss and vertigo
Summary Table:
| Test | Typical Findings in Otosclerosis |
| PTA | Conductive loss (low frequencies), Carhart notch at 2 kHz; mixed if cochlear involvement |
| VNG | Usually normal; mild vestibular weakness if labyrinthine involvement |
| ABR | Normal; wave I latency may be slightly prolonged if cochlear involvement |
| Symptoms | Mild, episodic vertigo; progressive conductive hearing loss; tinnitus possible |
Summary:
| Modality | Findings |
| CT | Best; shows demineralization of otic capsule/stapes area |
| X-ray | Limited; rarely used now |
| MRI | Usually normal; may help if sensorineural loss or cochlear involvement suspected |
Conclusion:
Labyrinthine otosclerosis, usually affecting the stapes footplate, leading primarily to conductive hearing loss. Rarely, if the otic capsule or cochlea is involved (cochlear otosclerosis), it can cause sensorineural hearing loss and vertigo.
✅Case 22:
56 year old male with:
- Vertigo (due to vestibular nerve involvement)
- Progressive sensorineural hearing loss (unilateral)
- Tinnitus
- Sometimes facial numbness or weakness if CN V/VII involved
- Imbalance or ataxia if brainstem/cerebellum compressed
- Summary Table:
| Test | Typical Findings |
| PTA | Unilateral sensorineural hearing loss (often high-frequency), reduced speech discrimination |
| VNG | Unilateral vestibular hypofunction, spontaneous or gaze-evoked nystagmus |
| ABR | Prolonged I–III or I–V interpeak latency, possible wave V absence |
| Symptoms | Vertigo, imbalance, tinnitus, possible facial numbness/weakness |
| Modality | Findings |
| MRI | Gold standard; shows tumor and brainstem/CPA involvement |
| CT | May show bony changes; not sensitive for small tumors |
| X-ray | Not useful |
Conclusion:
Small vestibular schwannoma may mainly present with vertigo and mild hearing loss, while a larger tumor compressing the brainstem may produce mixed peripheral/central VNG patterns, ABR delays, and more pronounced symptoms.
Location: Typically arises from the vestibular portion of the 8th cranial nerve (cranial nerve VIII) in the cerebellopontine angle (CPA), compressing the brainstem.
✅Case 23:
72-year-old female with:
- Sudden sensorineural hearing loss (SSNHL) – often unilateral
- Tinnitus – ringing or buzzing in the ear
- Aural fullness – sensation of pressure in the affected ear
- Distorted or reduced speech understanding – especially in noisy environments
Test reults:
- VEMP (both cVEMP and oVEMP): Normal
- Caloric test results: Normal
- vHIT: Normal
- Balance tests (Romberg, Fukuda, gait): Normal
- Pure-tone audiometry (PTA): Unilateral sensorineural hearing loss
- OAE: Absent or reduced on the affected side
Conclusion:
Pure cochlear neuritis (only the cochlear branch of CN VIII is inflamed).
- The lesion is only in the cochlear branch (hearing portion of CN VIII).
- VEMP (both cVEMP and oVEMP): Normal
- Because the vestibular pathways (saccule, utricle, semicircular canals) are intact.
- This helps differentiate cochlear neuritis from labyrinthitis or vestibular neuritis.
Typical Associated Features
- Recent viral infection (cold, flu, herpes simplex reactivation) often precedes neuritis
- Sudden onset (hours to days) rather than gradual
- No focal neurological deficits (if there are, it raises suspicion for central causes like brainstem stroke or MS rather than isolated neuritis)
✅Case 24:
28-year-old male with:
- Suspected occupational hearing loss.
- History and demeanor inconsistent with reported severity.
Test Results:
- PTA: Reported thresholds: ~60–70 dB HL across frequencies (suggesting moderate–severe loss).
- WRS (Word Recognition Score): Excellent at conversational levels,
- ABR: Robust, repeatable waveforms at normal or near-normal intensities (~20–30 dB nHL) with Absolute and interpeak latencies normal.
- OAEs: Present and robust DPOAEs/TEOAEs at multiple frequencies.
Diagnosis: Pseudohypacusis (functional/nonorganic hearing loss).
- PTA: Moderate–severe HL reported, but inconsistent and unreliable.
- Speech: Much better performance than PTA predicts (SRT too good, WRS excellent).
- ABR: Normal thresholds and latencies → normal auditory pathway.
- OAE: Present emissions → cochlear function intact.
✅Case 25:
Patient:
- 52-year-old male, complaint of recurrent vertigo, right-sided ear fullness.
Caloric Irrigation Results (water at 30° & 44°C, recorded in °/s):
| Irrigation | Right Ear (°/s) | Left Ear (°/s) |
| Warm 44°C | 6 | 18 |
| Cool 30°C | 5 | 20 |
Total Right Responses = 6 + 5 = 11°/s
Total Left Responses = 18 + 20 = 38°/s
Total Bilateral Response = 49°/s
Calculated Unilateral Weakness (Jongkees’ Formula):
UW=(Right+Left)/(Right−Left)×100
UW= (11−38)/49×100=−55%
Conclusion:
- 55% Unilateral Weakness (UW) in the Right Ear
- This indicates significant hypofunction of the right horizontal semicircular canal or vestibular nerve.
- Fixation suppression: normal.
- No directional preponderance.
Peripheral Vestibular Disorders that could cause unilateral weakness:
- Neuritis / Labyrinthitis
- Vestibular
- Ménière’s Disease
- Acoustic Neuroma (Vestibular Schwannoma)
- Chronic Otitis Media / Middle Ear Pathology
- Superior Canal Dehiscence (SCD)
